Welcome to the latest edition of our health insurer financial update, Pulse. We aim to keep you informed about key market trends and dynamics that impact health insurer financial results and profitability. Earlier this year we released Q1 financials and in July, we released our Summer 2024 edition, a comprehensive report covering 2023 reported statutory financials. This latest update contains Q2 2024 net income trends for insured business, earnings highlights, commercial and Medicaid membership (including redeterminations), and market capitalization highlights.
Six key trends in health insurance in Q2 2024
- Average profit margins increased but are below Q2 2023 levels. The average profit margin rose by 1.4% from Q1 2024, mainly due to UnitedHealthcare’s return to profitability, but is still 0.6% lower than reported in Q2 2023.
- Average loss ratios increase but CVS Health (Aetna) shows improvement. Average loss ratios increased from Q1 2024 due to higher acuity in the Medicaid business and are 1.6% higher than in Q2 2023. CVS Health (Aetna) reported a 0.8% loss ratio improvement compared to Q1 2024.
- Lower operating expense ratios contribute to profit margins.
- Medicaid membership continues to decline and remaining members have higher acuity after redeterminations. Medicaid membership declined further due to eligibility redeterminations, with some members moving to commercial products. By the end of Q2 2024, many insurers believed they were nearing the end of the redetermination process. They also indicated that remaining Medicaid membership has higher acuity than those who left in the redetermination process.
- Market capitalization reduction for Molina and CVS Health (Aetna). As of June 28, 2024, both Molina and CVS Health (Aetna) have lost more than a quarter of their market capitalization since the end of Q1 2024.
- UnitedHealthcare recognizes impact from Change Healthcare cyberattack. The Change Healthcare cyberattack is estimated to have cost UnitedHealthcare roughly $0.92 per share in Q2 2024 and is estimated to reduce full-year EPS by $1.90 to $2.05.
Net income for public health insurers improved compared to Q1 2024
Overall, the unweighted average profit margin (net income/premium) for the four insurers was 4.6%, which is 1.4% higher than the Q1 2024 unweighted average. However, it is 0.6% lower than the Q2 2023 unweighted average of 5.2%, driven by UnitedHealthcare’s decreased margins on its insured business relative to estimated 2021-2023 levels.
UnitedHealthcare recorded a net profit margin of 4.3% in Q2 2024, a 5.7% increase over Q1 2024. They continue to see negative impacts due to the sale of their South American business ($1.3 billion in Q2 2024) and have started to recognize costs related to the Change Healthcare cyber-attack ($0.92 per share in Q2 2024).
Cigna saw their margin slightly decrease in Q2 2024, from 8.0% in Q1 2024 to 7.5% in Q2 2024, but that is in-line with the Q2 2023 margin of 7.4%.
Elevance’s profit margin remained flat at 5.3% in the quarter and is 1.0% higher than the 4.3% Q2 2024 reported margin.
CVS Health (Aetna) saw their profit margin increased slightly in the quarter, from 0.9% in Q1 2024 to 1.3% in Q2 2024. The 1.3% margin reported in Q2 2024 is 1.9% lower than the 3.2% margin reported in Q2 2023.
Average loss ratios rose in Q2 2024 compared to Q1 and Q2 2023
On average, the medical loss ratios (medical costs/premium) for all four of the public large companies that we reviewed were 0.8% higher in Q2 2024 than Q1 2024. In Q2 2024, reported loss ratios were 89.6% for CVS Health (Aetna), 86.3% for Elevance, 85.1% for UnitedHealthcare, and 82.3% for Cigna.
Overall, the unweighted average loss ratio was 1.6% higher in Q2 2024 at 85.8% compared to Q2 2023 at 84.2%, as all carriers except Elevance increased year-over-year. The increases are: CVS Health (Aetna) (86.2% to 89.6%), UnitedHealthcare (83.2% to 85.1%), and Cigna (81.2% to 82.3%).
Average Q2 2024 operating expense ratios were the lowest reported since COVID
Operating expense ratios (operating expense/premium) decreased by 0.5% from Q1 2024 to Q2 2024. Cigna (-1.2%), Elevance (-0.1%), and UnitedHealthcare (-0.9%) all reported decreases, while CVSHealth (Aetna) increased slightly by 0.2%.
Most companies’ Q2 2024 utilization is on the high end of expectations, particularly for Medicaid business, as redeterminations leave companies with higher acuity members enrolled in Medicaid than prior quarters
Centene. Health benefits ratio for the quarter was 87.6% and 87.3% year-to-date, which puts them in the high end of the full year guidance of near 87.9%. Centene noted that Medicaid is driving up the health benefits ratio as the acuity of retained and rejoining Medicaid members is higher than the acuity of members lost during the redetermination process.
Cigna. Medical care ratio was within Cigna’s expected range in the quarter at 82.3%, including roughly 40 basis points attributable to unfavorable prior year Medicare Advantage risk adjustment recognized in Q2. Full-year medical care ratio (MCR) is expected to be in the range of 81.7% to 82.5%, the same range as reported in Q1. Additionally, Cigna expects their third quarter medical care ratio to be slightly lower than 83.1%.
CVS Health (Aetna). Reported medical benefit ratio of 89.6% in the quarter, which was 340 basis points higher than the prior year quarter. CVS Health’s (Aetna) Medicare Advantage utilization continues to run at elevated levels, and they saw higher acuity in current Medicaid membership because of redeterminations. CVS Health (Aetna) expects their 2024 medical benefit ratio to be between 90.6% and 90.8%, an increase of 80 to 100 basis points from previous guidance.
Elevance. Reported a benefit expense ratio of 86.3% within the quarter, showing a 10-basis point improvement year-over-year. This improvement was driven by premium rate adjustments and recognition of medical cost trends, disciplined medical management, and a shift in business mix towards commercial lines. Elevance expects their full-year benefit expense ratio to be in the upper half of their initial guidance range, in part due to higher Medicaid acuity driven by redeterminations.
Humana. Reported a benefit ratio of 89.5% for the quarter, which was lower than expected. This was due to favorable claims development and higher-than-expected revenue, but offset by higher inpatient costs, particularly towards the end of the quarter. Humana reaffirmed their previously communicated benefit ratio guidance.
Molina. Saw a business-wide medical cost ratio of 88.6% for the quarter, and the year-to-date MCR is also 88.6%. Molina’s Medicaid business had a 90.8% MCR for the quarter, 0.7% of which is attributable to a one-time retroactive premium item in their California business. Excluding the one-time item, the 90.1% Medicaid MCR is still high relative to historical ratios, partially driven by higher acuity of remaining members after redeterminations. Medicare Advantage saw a favorable quarterly medical cost ratio of 84.9%, primarily due to favorable risk adjustment results as well as benefit adjustments implemented for 2024. The medical cost ratio for Molina’s Marketplace business was 71.6% in the quarter, also favorable to expectations.
UnitedHealthcare. Reported a medical care ratio of 85.1% for the quarter. This reflects a roughly 25 basis point increase related to regulatory action in Chile and a 40 basis point increase due to the suspension of some care management activities due to the Change Healthcare cyberattack. UnitedHealthcare reported three other adverse impacts to their medical care ratio: 1) Member mix within Medicare Advantage and dual special needs plans; 2) A timing mismatch between the health status or remaining Medicaid members and state rate updates; and 3) Lingering upshifts in provider coding intensity. Like Q1, UnitedHealthcare did not reflect any favorable earnings impacting medical reserve development in the quarter, and they will continue to monitor the impact of the cyberattack and the additional $800 million of claims reserves booked in Q1.
Medicaid membership continues to decline, while commercial enrollment grows
In Q2 2024, total Medicaid membership for public carriers decreased by 1.7% from Q1 2024, driven by the continued redetermination of Medicaid eligibility. However, total Medicaid enrollment is still about 23% higher than at the beginning of the pandemic. Total commercial membership increased roughly 0.4% over Q1 2024, as some individuals who lost Medicaid coverage were able to shift to commercial coverage.
During their earnings calls, most carriers provided insight into their year-to-date membership performance. In addition, some carriers also commented on the ongoing process of states redetermining Medicaid eligibility. The public health emergency officially ended on May 11, 2023, with several states beginning the redetermination process on April 1, 2023.
Centene. The quarter ended with approximately 13.1 million Medicaid members, slightly lower than expected. Commercial business saw slight growth of about 50,000 members to 4.8 million members.
Cigna. The first quarter ended with approximately 19 million medical customers, representing a reduction of 0.2 million members since the end of Q1 2024.
CVS Health (Aetna). The quarter concluded with a medical membership of nearly 27 million, primarily reflecting growth in Medicare and individual exchange business.
Elevance. They ended the quarter with medical membership of approximately 45.8 million members. This reflects attrition in Medicaid, of which they believe that nearly all their Medicaid members have already had their eligibility redetermined. Elevance added 354,000 commercial fee-based members year-over-year.
Humana. The quarter ended with approximately 16.3 million members, an increase of roughly 100,000 from Q1 2024. Humana’s membership growth in Medicare Advantage is higher than expected, and they raised their membership forecast by 75,000 members.
Molina. In the quarter, Molina’s Medicaid enrollment decreased by 100,000 members due to the net impact of Medicaid redeterminations. So far, Medicaid enrollment is down 650,000 because of redeterminations. Due to timing of reconnects, Molina ultimately expects to regain roughly 50,000 of membership lost due to redeterminations in the second half of the year. Overall, they’ve been able to transfer roughly 40% of the lost Medicaid enrollment into their marketplace products.
UnitedHealthcare. UnitedHealthcare added 2.3 million new domestic commercial members in the first half of the year. Medicaid business ended the first quarter with 7.4 million members, a 270,000 decrease from the end of Q1 2024 reflecting attrition due to Medicaid redeterminations.
The chart below displays the changes in reported enrollment for the 16 most recent quarters for commercial and Medicaid for a set of public companies where counts were available on a consistent basis. In the quarter, total commercial membership increased by about 0.4 million, while Medicaid membership decreased by approximately 0.7 million in the quarter due largely to the eligibility redetermination process.
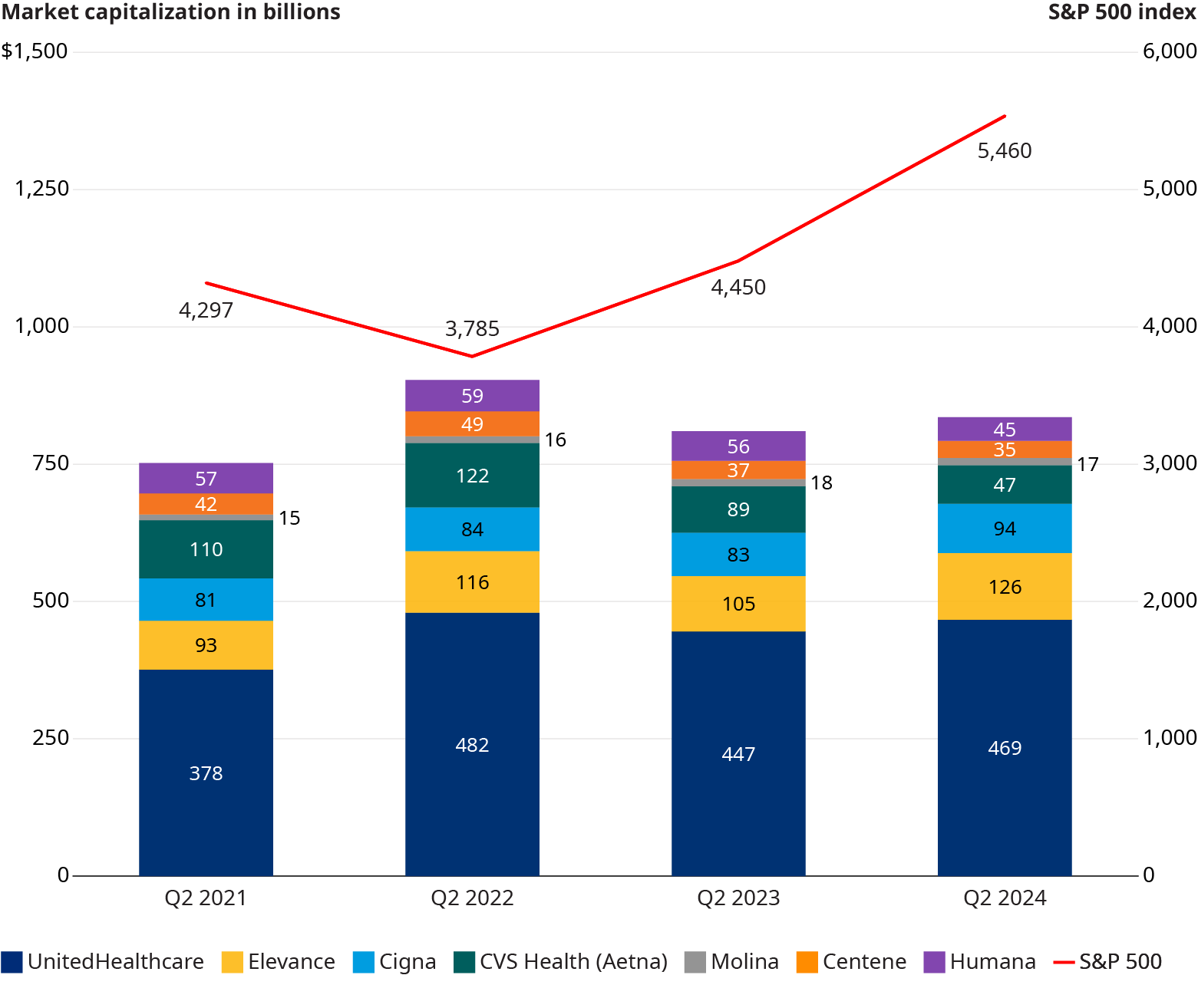
Health plan capitalization rose over the year but trailed the S&P 500 Index in Q2 2024
From Q2 2021 to Q2 2024, the collective market capitalization of the seven public healthcare companies we monitor experienced modest growth. Between June 30, 2021, and June 28, 2024, the combined market capitalization of these seven public health plans rose by 10.8%. During the same period, the S&P 500 index grew by 27.1%, outpacing the healthcare companies by 16.3%. However, despite the substantial overall gain by the health plans, there was a noticeable divergence in market capitalization of healthcare firms compared to the S&P 500 Index in the last quarter. From Q1 2024 to Q2 2024, the market capitalization of the seven public companies dropped by 3.1%, while the S&P 500 index increased by 3.9% over the same period.
Healthcare stocks showed significant variation in Q2 2024 returns
Humana (+7.7%) and Elevance (+4.4%) both outpaced the S&P 500 Index (+3.9%). Molina (-27.6%), CVS Health (Aetna) (-26.1%), and Centene (-15.7%) both shed over 10% of their market capitalization in Q2 2024. Cigna also dropped in Q2 2024, with an 8.8% decrease in market cap in the quarter. UnitedHealthcare regained some of their Q1 2024 share price losses in Q2 2024, with a modest 2.8% increase.
Look out for the Pulse Q3 2024 financials in the next quarter.