Prior authorization programs are management processes used by insurance companies to determine if a prescribed product or service will be covered. They can reduce total cost of care (TCOC) while ensuring that evidence-backed clinical protocols are followed. However, they also have a tradeoff: they can create administrative burdens and care delays for both members and providers.
This process can hurt the health plan’s net promoter scores (NPS) from members and providers. For Medicare Advantage plans, this can also affect the CAHPS survey results and lower star ratings. Health insurance carriers who do not act quickly risk falling further behind these large payers who have already taken steps to simplify their prior authorization programs.
UnitedHealthcare has recently announced that they were significantly reducing the number of services subject to a prior authorization process. In the coming months and years, it will be necessary to reduce the negative impacts of prior authorization and improve the health care experience for both consumers and providers by identifying opportunities and modernizing the process.
Healthcare leaders weighing in on prior authorization
Recently, two of the biggest healthcare payers, UnitedHealthcare and Health Care Service Corporation (HCSC), have made announcements on significant changes to their programs. HCSC has recently expanded its use of artificial intelligence (AI) to review and approve prior authorization submissions in a more automated workflow. The company expects to greatly reduce the time it takes to review these submissions by using this technology.
Challenges streamlining prior authorization
There are many challenges which make it difficult for a carrier to simplify its prior authorization program. The processes and datasets are often messy, complicated, and disjointed. Multiple teams and vendors may be running segments of the program in silos. Legacy processes and systems may not be maintained over the years and can even become obsolete. This makes it challenging for clinical leadership (CMOs), operational leadership (COOs), and compliance areas to design analytics and derive insights to evaluate the effectiveness of the overall program.
Using predictive modeling and data science techniques, Oliver Wyman’s Actuarial team can help payers evaluate their existing prior authorization process. Oliver Wyman helps clients identify opportunities to modernize their prior authorization process to reduce operational costs, improve health outcomes, remove unnecessary barriers to care, and improve the member and provider experience.
Oliver Wyman’s proprietary data enrichment pipeline allows disparate data sources, including prior authorization data, claim data, and provider data, to be seamlessly brought together. A data lake, which contains national benchmarks for the Affordable Care Act (ACA), commercial, and Medicare populations, is then utilized to make comparisons to the client’s existing program. This allows for the entire prior authorization process to be visualized and analyzed in a holistic view so areas of opportunity can be identified and targeted for strategic improvements.
Improving the prior authorization process
Different predictive models can be leveraged to improve the prior authorization process. Some examples include:
- Observing which services do or do not need to be subject to a manual or automated prior approval process
- Determining which members and providers are the most sensitive to the negative impacts of the existing prior authorization process
- Simulating the impact of proposed changes on operational and medical costs
- Modeling the impact of prior authorization denials on risk scores and HEDIS measures
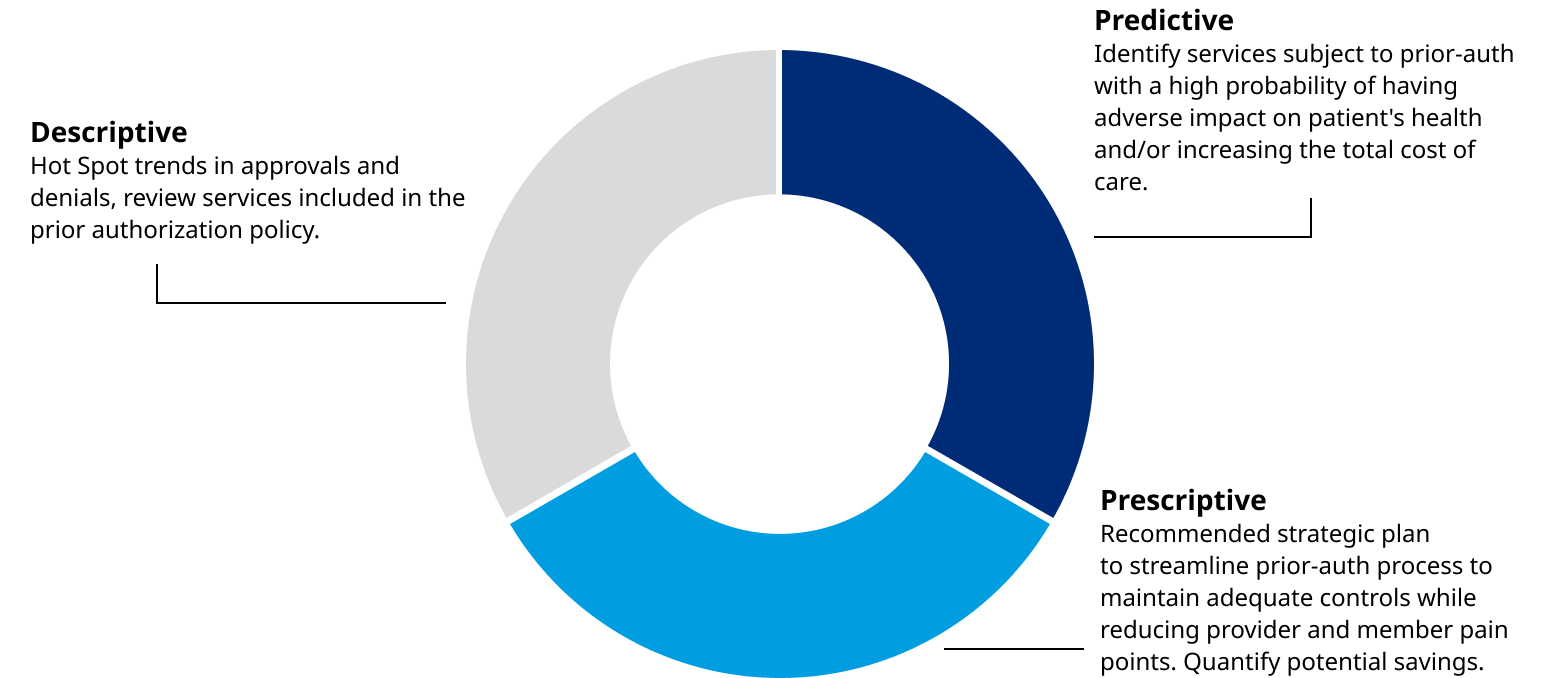
When was the last time you reviewed your prior authorization program? Are you able to effectively measure the value the program delivers? Are you certain your program is not adding excess operational costs to your firm and unnecessary burdens on your members and providers? It is clear from recent market trends that some carriers are asking these questions and have taken strong actions to improve their prior authorization programs. If you need help keeping pace with this market trend, the Oliver Wyman team has a plan to help you. The key to this process is Oliver Wyman’s best practice approach to problem solving which combines descriptive and predictive analytics to create lasting strategic solutions to address the needs of our clients.