California’s Medicaid, known as Medi-Cal, is a far-reaching safety net program that covers one in three Californians, half of California’s births, more than half of school-age children, and more than two-thirds of patient days in long-term care facilities. Building on the positive outcomes of Health Homes Program and Whole Person Pilot, in early 2022, the Department of Healthcare Services (DHCS) launched a new statewide initiative called California Advancing and Innovating Medi-Cal (CalAIM) to transform Medi-Cal with a special focus to address social drivers of health and expand access to coordinated person-centered care.
Two critical components of CalAIM
- Enhanced Care Management (ECM) — A new required benefit available to highest-need MCP members. These members meet one of the criteria of “population of focus” which includes individuals and families experiencing homelessness, adults at the risk of institutionalization and eligible for long-term care and patients with complex clinical needs. Furthermore, there are opportunities to negotiate value-based care with ECM providers to achieve improved financial results and ultimately better health outcomes for the population. These ECM providers have a “boots on the ground” approach to patient engagement and are staffed with Community Health Workers, Licensed Clinical Social Workers (LCSW) and registered nurses.
- Community Supports (CS) — A new optional service provided to MCP members. Although these services are optional, the MCPs are strongly encouraged to offer them. Such services include housing transition navigation services, housing deposits, short-term post hospitalization housing, respite services and others.
Market challenges in Medicaid plans
A key feature of ECM is that MCPs are responsible for identifying and enrolling who meet the eligibility criteria. This means meeting enrollees wherever they are – in homeless encampments, in a shelter, in their doctor’s office, or at home. This poses new challenges to the plans, the first being identifying the eligible members. As the criteria for population of focus are broad and extend to social and behavioral risk factors, MCPs must go beyond traditional enrollment channels.
Using proprietary Oliver Wyman Analytics to predict risk
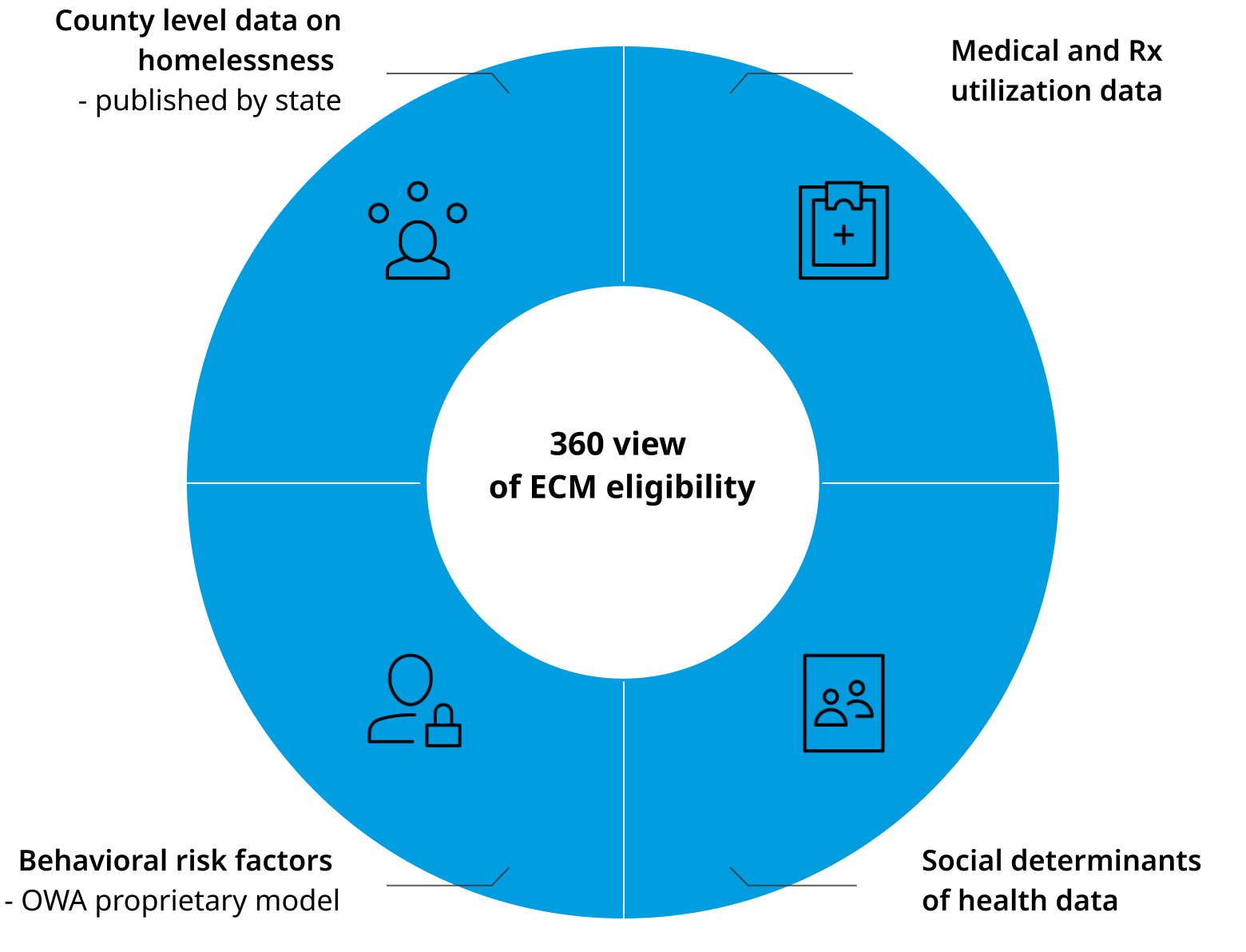
The Oliver Wyman Actuarial team supplements MCPs eligibility and health care utilization data with social determinants of health (SDoH) data and proprietary predictive model to predict behavioral health risk and identify the highest-need patients. This can also supplement the referrals from community-based organizations in identifying eligible patients for ECM. The person level SDoH data along with county level demographic data on homelessness published by California’s Homeless Data Integration System (HDIS) is used to validate the population identified to be at high risk of homelessness.
Tools for success under CalAIM
Early identification and person-centered care, along with addressing social risk factors such as access to food, housing and transportation is likely to have a transformative impact on the patients’ lives and should bring down the cost of care. By monitoring ROI on interventions, the plan can allocate the resources effectively and succeed under CalAIM.